by Nicole L. Fice, Cory E. Goldstein, and Austin R. Horn
The media response to the recent Zika virus outbreak has been sensationalized and, as a result, governmental responses have been largely misplaced. Zika is a virus that has been around for decades, with relatively mild symptoms. However, a recent outbreak in Brazil that coincided with 2016 Summer Olympics in Rio De Janeiro has put Zika in the global spotlight. Media attention has focused almost exclusively on Zika’s association with microcephaly, a condition whereby infants of infected mothers are born with small heads and sometimes have related developmental issues. Public prevention campaigns have also focused disproportionately on women, urging them to be especially diligent in avoiding or delaying pregnancy. This places the majority of the responsibility of eradicating Zika on women. Yet, this is misleading as it misidentifies the relevant issue; insofar as the aim is to mitigate the spread of Zika, the most expeditious means of doing so is the eradication of the Aedes aegypti mosquito that carries the virus.
The Zika controversy, i.e. the plethora of responses from various agencies, brings to light broader questions regarding women’s reproductive rights. Responses arising from reproductive rights discourse is helpful in refocusing discussions about rights of women. But, these responses have almost entirely been focused on access to abortion services and regulations. However, other major systemic issues that Zika exemplifies have not been addressed. For instance, poverty in the context of the Zika controversy affects people in two ways, first by impacting their reproductive rights, and second by exposing them to mosquitos. Thus, we should utilize a framework of reproductive justice when talking about the effects of Zika.
§1. Zika: virus, media coverage, and governmental response
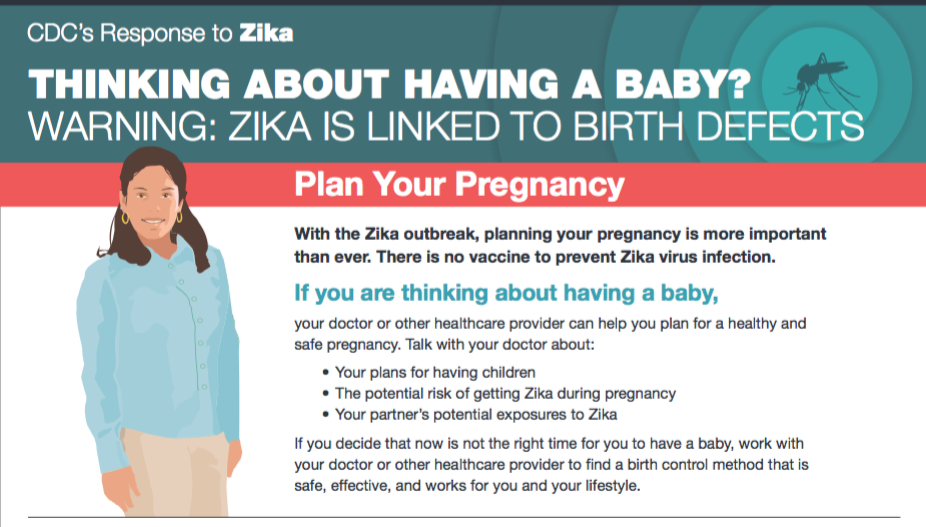
According to the Centre for Disease Control and Prevention (CDC), the 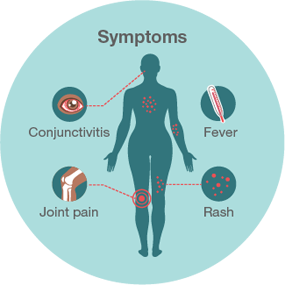 Zika virus is a mosquito-borne infection transmitted through bites from the Aedes aegypti, i.e., the yellow fever mosquito. The virus can also be transmitted from a pregnant woman to her fetus, through sexual intercourse, and blood transfusion. However, many people infected with Zika will not exhibit symptoms or will have only mild symptoms. Common symptoms (image via CDC) include: fever, rash, joint pain, conjunctivitis (red eyes), muscle pain, and headache; other symptoms may manifest in fetuses and infants whose mothers were infected with Zika during pregnancy, such as defects of the eye, hearing deficits, and impaired growth.
Zika virus is a mosquito-borne infection transmitted through bites from the Aedes aegypti, i.e., the yellow fever mosquito. The virus can also be transmitted from a pregnant woman to her fetus, through sexual intercourse, and blood transfusion. However, many people infected with Zika will not exhibit symptoms or will have only mild symptoms. Common symptoms (image via CDC) include: fever, rash, joint pain, conjunctivitis (red eyes), muscle pain, and headache; other symptoms may manifest in fetuses and infants whose mothers were infected with Zika during pregnancy, such as defects of the eye, hearing deficits, and impaired growth.
Zika infection during pregnancy has also been associated with microcephaly. Microcephaly — literally meaning ‘small-headed’ — is a birth defect that affects the growth of a fetus’ head. Babies born with microcephaly often have smaller brains, which may lead to developmental delays, such as problems with speech development, motor development, and intellectual disabilities. Microcephaly also ranges in severity. In mild cases, a child with microcephaly might not experience any of these symptoms, and may otherwise lead a healthy life. In more severe cases, a child’s life may be threatened. Although Zika has caused an increase in cases of microcephaly, there can be several other associated causes, including rubella, exposure to harmful substances, antenatal alcohol ingestion, and certain drugs.
The Zika virus was first discovered in the Aedes aegypti mosquito in 1947, with the first human cases of infection occurring in 1952. In the mid-1930s efforts began to exterminate the Aedes aegypti mosquito (largely owing to other, comparatively more serious, mosquito-borne viruses, such as malaria, yellow fever, dengue fever, and chikungunya), and by the mid-1960s several countries announced they had eradicated the mosquito. The initial success of the efforts resulted in less attention to the mosquito and dwindling funds for their extermination, meaning that efforts were eventually abandoned. Hence, it did not take long for mosquito-borne diseases to reemerge.
Over the past several decades sporadic outbreaks of Zika have occurred globally, primarily in the southern hemisphere (Africa, Southeast Asia, and the Pacific Islands). Only recently, however, have higher instances of microcephaly in Latin America been associated with Zika, largely due to the recent outbreak in Brazil. For instance, the worst affected state in Brazil, Pernambuco, has experienced a 30 percent increase in rates of microcephaly since 2010. This translates to approximately one to two percent of newborns being affected by microcephaly in the worst-hit areas in Brazil (see Reuters article). Those most affected by Zika and microcephaly are women and men living in poverty. Because of increased cases of microcephaly, the World Health Organization (WHO) declared the outbreak in Brazil a public health emergency on February 1st, 2016.
While it is evident that Zika has been around for several decades, media coverage of the most recent outbreak in Brazil has been sensational, fuelled primarily by the 2016 Summer Olympics in Rio De Janeiro. A Harvard Public Health Review recommended that, due to the Zika outbreak, the Olympics should be postponed. The article perpetuates the sensationalization of Zika by criticizing the International Olympic Committee and the WHO for calling Zika a “manufactured” outbreak. The general media responses have run with headlines such as, “Rio 2016: Olympic Games poses ‘unimaginable risk’ of spreading the Zika virus, Australian expert warns.” Headlines such as these are dangerously misleading, ahistorical, and contribute to a sense of global panic completely unsupported by fact.
Governmental responses to Zika have also failed to accurately identify the pertinent issue, and thus mitigation efforts have been largely misplaced. Billions of dollars in global aid and state-sponsored research funding have been diverted from more urgent global pandemics to Zika eradication efforts. For instance, tropical diseases such as malaria, yellow fever, dengue fever, and chikungunya affect a disportionate number of people worldwide, enjoy a much greater ease of transmission, and are associated with symptoms and prognoses substantially more severe than the Zika virus. Moreover, the primary focus of media and governmental attention has not been on the Zika virus itself, or the Aedes aegypti mosquito that carries the virus (and a host of others), but rather on one of its associated symptoms: microcephaly.
Media and governmental responses (see On the Media podcast) have placed an undue amount of the responsibility for preventing Zika — and thus microcephaly — on women. For instance, women have been targeted disproportionately by various public advertisement campaigns, which urge women to avoid standing water, wear mosquito repellent and full-length clothing, and to stay indoors. Perhaps most unsettling of these recommendations are those that urge women to delay pregnancy. El Salvador has, for example, urged women to avoid pregnancy until 2018 in response to the spread of Zika. Other countries, like Colombia, have made similar suggestions. The WHO also suggested that women in areas affected by the Zika virus delay pregnancy. The responsibility of men in preventing the spread of Zika, and thus microcephaly, has been all but completely overlooked — as if immaculate conception were a regular occurrence. Moreover, by placing the burden of prevention on women the media has also overlooked the critical role of governments in mitigating the spread of Zika, such as renewed efforts to eradicate the Aedes aegypti mosquito — which carries a slew of deadly viruses — and, equally important, providing safe and convenient access to abortion and contraception. Asking women to simply “avoid” contracting Zika while pregnant is not only misleading, in that it misidentifies the most effective prevention strategy — i.e., mosquito eradication — but it also places undue emphasis on women’s role in mitigating the spread of Zika. Urging women to avoid or delay pregnancy, while simultaneously barring access to safe and effective contraceptive measures, raises an issue of much greater social importance than a virus that has been around for decades, and has symptoms akin to the common cold; namely, women’s reproductive rights.
§2. Reproductive rights for the case of Zika
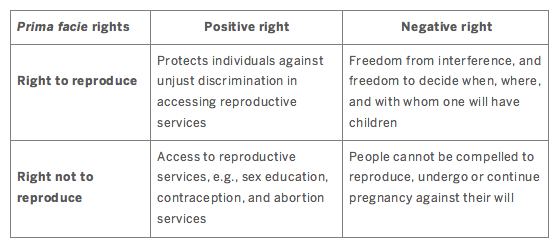
In Why Have Children? The Ethical Debate, Christine Overall proposes that reproductive rights can be split into two prima facie rights: (i) the right to reproduce, and (ii) the right not to reproduce. Both prima facie rights have a corresponding positive right and negative right.
The case of Zika, and the governmental responses to its outbreak in Latin America, highlights the need for a discussion about the reproductive rights of women in the countries most affected. In applying Overall’s reproductive rights framework to Zika, we argue that the case of Zika, and the governmental responses, clearly violates three of these rights: (i) the positive and (ii) negative right to reproduce, and (iii) the positive right not to reproduce.
Women have a positive right that protects them against unjust discrimination in accessing reproductive services, such as antenatal and neonatal care, or child benefits. The positive right to reproduce is infringed by governments’ current responses to Zika mitigation efforts, which tend not to include things like adequate child benefits. Women who contract Zika during pregnancy, and go on to have children with microcephaly, have trouble receiving assistance from the government. Debora Diniz writes,
“Some news reports have included accounts of women being abandoned by their partners after the birth of a baby with neurological problems. The state shouldn’t abandon them, too. It needs to provide financial support and social services for poor women and their children who are suffering from the effects of Zika.”
Women in poverty, who are disproportionately affected by Zika, might struggle with the high costs of caring for a child with microcephaly. Brazil’s government does offer assistance, but it can be difficult to obtain.
The negative right to reproduce is a freedom to decide when, where, and with whom someone has biological children. The government and WHO responses that urge women to delay pregnancy for upwards of two years is a clear violation of the negative right to reproduce, as women are not free to decide when to have children.
The positive right not to reproduce ensure that women (and men) have access to reproductive services for women, such as sex education, contraception, and abortion services. This right has received some attention in the media and in academic circles. As mentioned above, Brazil and other countries in Latin America have very strict laws that limit access to abortion and other reproductive services. The limited access to these services violates women’s positive right not to reproduce. Diniz mentions that wealthy women in Brazil can pay to have safe and effective abortion services, while poor women resort to unsafe abortions. However, as Alexandra Minna Stern points out, many women with strong religious beliefs might choose to not terminate pregnancies even if the fetus has mild to severe microcephaly. Thus, women should be able to make a decision about whether to terminate or continue a pregnancy, and this entails that all women — not just the wealthy — ought to have access to safe and effective reproductive services.
Diniz, who advocates for better access to reproductive services in Brazil, argues that “asking women to avoid pregnancy without offering the necessary information, education, contraceptives or access to abortion is not a reasonable health policy.” Bioethicists and other scholars in Latin America have sparked a global debate on access to reproductive services. Scholars argue that certain regulations infringe on women’s reproductive rights, and need to be changed; however, we should not limit our discussion to abortion.
§3. Reproductive justice for the case of Zika
There is no doubt that discussions about reproductive rights are important; however, we believe that the focus on reproductive rights is, in some respects, too narrow in scope: it centres the discussion on abortion services and regulation. The responses from the reproductive rights movement do not sufficiently address how women in poverty, women of colour, and women in rural areas have limited choice, owing to a system that perpetuates poverty. For instance, women in these demographics often do not have access to adequate education and health care, and are the victims of racial profiling and systemic oppression. The reproductive rights movement also tends to focuses on choice. But, as the reproductive justice framework makes clear, often the choices of marginalized women are limited due to a lack of access to reproductive goods and services. Reproductive justice is therefore about more than simply advocating for the reproductive rights of marginalized women, it also addresses issues of access, and ending reproductive oppression caused by systematic inequalities. Reproductive justice brings those who are most vulnerable to the center of discussions. We believe that reproductive justice can more adequately address these broader systemic issues.
The reproductive justice movement arose as a response to what was (and currently is) overlooked in the reproductive rights movement. Sistersong is a network of social justice advocates attributed with the initial development of the concept of reproductive justice. According to Luna and Lurker, “reproductive justice […] emphasizes how reproduction must be considered among an array of social justice concerns [and…] is equally about the right to not have children, the right to have children, the right to parent with dignity, and the means to achieve these rights.” It is evident that reproductive justice is related to reproductive rights, as it incorporates the rights outlined by Overall. However, it adds an important third right: namely, the right to “parent with dignity.” This right evolved out of historical and contemporary threats to marginalized individuals’ — especially women’s — right to parenthood. These rights, viewed from a lens that takes seriously the oppressive forces that impact the lives of marginalized women, are foundational to the enterprise of reproductive justice.
The reproductive justice framework allows us to clearly view the systemic issues raised by the Zika controversy. Women receive insufficient assistance while raising children with microcephaly, and therefore the right to parent with dignity in an affirming and supporting environment is violated. Women should be given control over their reproductive lives, and this entails that all women should have access to various reproductive goods and services—including better support for women who have children with microcephaly. Reported cases of microcephaly are forgotten after headlines are published, and women are left to bear the brunt of the responsibility in caring for children with microcephaly (Stern). Support needs to be strengthened for these women and their families. However, systemic inequalities also impact the reproductive and parental lives of marginalized women, and underlie issues of access and social support.
The media coverage and governmental response to the recent Zika outbreak misidentifies the relevant issue to mitigation efforts, and, consequently, places undue responsibility on women. As a result, the rights of women, and marginalized women in particular, have been violated. But these violations are also influenced by systemic issues of inequality and oppression are external to the Zika controversy. The people affected by the Zika virus are disproportionately marginalized, and this includes rural women, women of colour, and women living in poverty. These marginalized demographics are left without access to safe abortions or contraception and they often do not receive adequate support from the state. They are also left without access to various social goods, such as adequate wages and safe environments to house their families. As Stern writes: “Zika underscores the depth of inequalities related to race, poverty, and gender, and the need for comprehensive and holistic reproductive justice”. To alleviate these effects of the Zika virus, felt most strongly by marginalized peoples, we need to address intersecting oppressions that cause unequal access and inadequate support. The reproductive justice framework makes it clear that we need to bring the most marginalized of voices to the centre of the discussion about Zika. Focusing on those who are least able to exercise their rights, and providing them the means to actualize those rights, will ensure that everyone will have the ability to do so.
Reframing the discussion on the Zika controversy in terms of reproductive justice highlights questions regarding women’s reproductive rights and broader systemic issues. A proactive, justice-oriented response to the Zika virus should not only be aimed at mosquito eradication, but also aimed at reducing systemic inequalities that cause the virus to disproportionately affect marginalized women in a variety of ways. We echo Diniz’s poignant remarks:
“In the short term, the government needs to control the mosquitoes by destroying their habitat and working with the international community to advance knowledge about how to stop the disease. But that’s only a start. Women need to be given the power to manage their own pregnancies.”
Pictured above: Zika plan your pregnancy poster (via CDC)